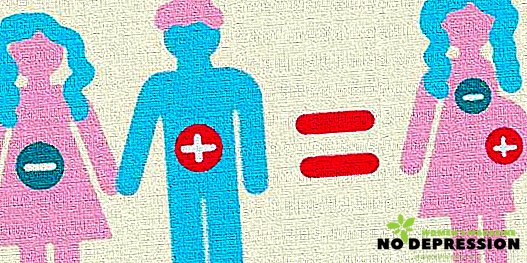
Many couples are not even aware of such a concept as rhesus conflict. Almost no one is interested in this phenomenon in everyday life, since it does not carry a negative impact.
But rhesus-conflict during pregnancy is quite dangerous and can cause the development of various pathologies. This situation takes place when the rhesus of the parents do not fit together much.
What is rhesus-conflict during pregnancy
First you need to explain, but what is the Rh factor in general? Rh factor - a protein located on the surface of blood cells, that is, red blood cells. This protein has people with positive rhesus, with negative it is absent.
Rhesus conflict during pregnancy is a phenomenon in which the expectant mother has a positive Rh, and the fetus is negative. The conflict occurs directly between the pregnant woman and the fetus.
As a rule, the conflict does not occur in the first pregnancy, but in subsequent ones. Despite this fact, it often happens that such a phenomenon occurs in a primipara woman. It is believed that the incompatibility at the first childbearing is the safest, since the immune response is not so strong.
When and why does rhesus conflict
Rhesus-conflict is possible only in two cases: during transfusion of incompatible blood and during pregnancy. For the occurrence of this incompatibility during pregnancy, you must:
- the fetus must have positive blood, that is, inherit it from the father;
- The future mother's blood should have antibodies to the D-protein, in science this is called sensitization.
Of course, the main cause of incompatibility is the different Rh factor of the mother and the ovum. Still, some experts on this subject there is an opinion that highlights several additional causes of Rhesus conflict.
This theory is based on the fact that the production of antibodies was provoked by previous pregnancies, regardless of how they ended. What is important is the fact that the meeting of maternal blood with the blood of the fetus took place.
The reasons could be the following:
- Previous genera.
- Caesarean section.
- Surgical or medical abortion.
- Miscarriage in early pregnancy.
- Ectopic pregnancy.
- Premature detachment of the placenta.
It should also be noted that the development of this is possible if the expectant mother in the past was exposed to medical procedures that are carried out through the body’s natural barriers (skin, mucous membranes). The most striking example of this is any injection.
Rhesus-conflict during pregnancy: table
In order to avoid conflict, a woman planning to carry a baby should know the rhesus of her chosen one. According to statistics, there is a discrepancy between Rh-negative woman and Rh-positive man in 70% of cases.
In the table below, you can see the likelihood of incompatibility during pregnancy.
| Rh factor | |||
|---|---|---|---|
| Mother | Father | Child | Probability of incompatibility |
| positive | positive | 70% positive 30% negative | not |
| negative | positive | 50% positive 50% negative | high |
| positive | negative | 50% positive 50% negative | not |
| negative | negative | 100% negative | not |
It is known that there is a myth among the people that the onset of pregnancy is impossible between spouses with different Rh factors. This opinion is undoubtedly wrong.
How does Rh-conflict during pregnancy: symptoms
Clinical symptoms of incompatibility between the future mother and the fetus are absent. This phenomenon is a pregnant woman unable to diagnose on their own. Symptoms of conflict is detected by ultrasound.
Signs of violation are:
- swelling and thickening of the placenta;
- increase in fetal body size;
- increased liver and spleen size;
- violation of the pose of the baby, that is, his legs are retracted to the sides;
- the contour of the baby's head becomes double, which speaks of edema;
- fluid is visualized in the cardiac pouch and chest of the fetus.
If you identify the above symptoms in the study, the doctor makes a diagnosis such as hemolytic disease, which will occur in a child after birth.
Hemolytic pathology has 3 forms of flow:
- Edematous.
- Anemic.
- Icteric
The most severe form is considered to be edematous. A baby having this form of the disease is characterized by the presence of diminished reflexes, seizures, and vomiting.

Diagnostics, analyzes, research
Pregnant women who have an incompatibility with the fetus, are more sensitive control specialists. They are regularly sent for testing and ultrasound. Careful diagnosis is understandable, doctors try to prevent the development of pathologies or various kinds of complications, as well as to determine the most favorable period of delivery.
Diagnostic methods include:
- Blood test for antibodies. This procedure is scheduled once a month and determines the dynamics of antibody titer.

- Ultrasound. With this study, experts control the size of the fetus and its internal organs, as well as monitor the condition of the placenta.
- Doppler. This diagnostic method allows you to evaluate the work of the heart in a child and find out the speed of blood flow in large vessels.
- Cardiotocography. With its help, the doctor determines the presence or absence of fetal hypoxia.
- Amniocentesis. This procedure consists in collecting a small amount of amniotic fluid to assess the normalization of bilirubin in the fetal blood.
It should be noted that amniocentesis is a procedure that is performed by interfering with the natural barriers of the body of a pregnant woman.
This diagnostic method may have adverse consequences, so the expectant mother must give her written consent to conduct such a study.
Pathology treatment methods
Currently, obstetrics has proven the effectiveness of only one method of treatment of this pathology, it is intrauterine blood transfusion. This method of treatment can significantly improve the course of pregnancy, that is, reduce the risk of premature birth and the development of hemolytic disease.
 It is important to remember that this kind of therapy is carried out in the hospital under the supervision of several specialists at once. Also, the above treatment is carried out only at the 20th week of pregnancy or later, but not earlier than the specified period.
It is important to remember that this kind of therapy is carried out in the hospital under the supervision of several specialists at once. Also, the above treatment is carried out only at the 20th week of pregnancy or later, but not earlier than the specified period.
In addition to intrauterine blood transfusion, there are other healing methods that are practically not used in medicine. Their inefficiency is proven, and they also have a very strong effect on the immune system of the expectant mother.
These include:
- immunoglobulin treatment;
- transplanting a pregnant woman to the epidermis of the child’s biological father;
- desensitizing therapy.
Despite the scant list of treatment options for pathology, the correction of the fetus is making great strides.
Rhesus conflict delivery
Of course, the most effective way to stop the delivery of maternal antibodies to the fetus is delivery. In the last trimester of pregnancy, the increase in the number of antibodies reaches a maximum limit. In this case, experts prescribe delivery before the appointed time.
The method of delivery is strictly individual, as it depends on the duration of pregnancy and the condition of the child.
Delivery can take place in two ways:
- Cesarean section. In most cases, experts are inclined to this method, since it is more benign for the fetus with the established Rh-conflict.
- Natural childbirth. This method is permitted when the gestation period is over 36 weeks and the condition of the fetus is satisfactory in all respects.
It is worth remembering that vaginal delivery takes place under careful monitoring and compliance with recommendations for the prevention of intrauterine hypoxia. In cases where the condition of the woman in labor or the child is at risk, an emergency caesarean section is performed.
Possible risks, complications and consequences for the child
As mentioned above, specialists pay special attention to patients who have such a diagnosis as Rh-conflict. Close control is due to the fact that this pathological condition has many complications and negative consequences for the child.
Possible risks include:
- miscarriage in early pregnancy or fetal death;
- the development of hemolytic disease in the newborn;
- oxygen starvation of the child in the womb;
- a significant decrease in hemoglobin in the newborn;
- disruption of the kidneys, heart, liver and brain of a child.

Despite the above threats, expectant moms should not panic. Thanks to the implementation of all recommendations of the attending physician, 90% of cases of Rh conflict have a favorable outcome.
The conflict of the Rh factor in the second pregnancy
In most cases, the question of the occurrence of Rh-conflict in the second pregnancy arises directly in its occurrence, or preparing for it. With the occurrence of a second pregnancy, the expectant mother with negative rhesus should be well aware of the issues that carry information about the complications and risks of incompatibility.
You can determine the risk of conflict, based on the following data:
- After miscarriage, the probability of incompatibility is 3%.
- After artificial termination of pregnancy, it is equal to 5%.
- After a successful birth, it reaches 20%.

Rhesus-conflict in the second childbearing is considered not only the most common, but also quite dangerous. The fact is that during the second pregnancy, antibodies, as a rule, multiply at an elemental rate.
In this case, the expectant mother urgently goes to the hospital, where she undergoes an ultrasound examination and passes the analysis to assess the amniotic fluid.
Preventive measures
Far from the last place in this issue are prevention measures. It is their compliance that significantly reduces the development of incompatibility between the mother and the child during the second pregnancy.
Preventive measures are as follows:
- women with a negative Rh factor, you need to make every effort to save the first pregnancy;
- blood transfusion should be carried out taking into account the blood of the woman and the donor;
- the introduction into the body of a woman antiresus immunoglobulin after the first birth or abortion.

Women who plan to carry the child, just need to take into account the above recommendations. Do not let this pathological condition take its course, since with uncontrolled childbearing, the future mommy can achieve very disastrous consequences.
Summarizing, we can say that Rhesus-conflict is not a sentence, but it has a considerable number of complications and risks for an unfavorable outcome. Incompatible couples should take family planning as a whole very seriously. A pregnant woman should undergo a scheduled diagnosis in a timely manner and follow all the recommendations of a specialist.
Additional information about the Rhesus conflict is in the next video.