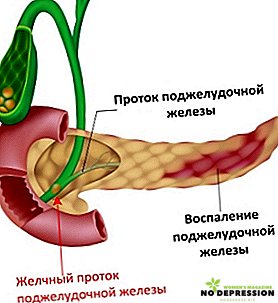
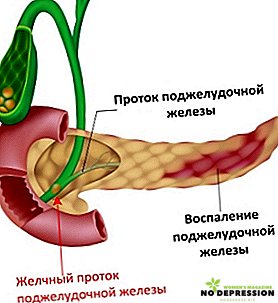
One of the most important organs of the gastrointestinal tract is the pancreas. It is in it that digestive enzymes are formed that break down proteins, fats and carbohydrates.
Her insular apparatus secretes insulin and glucagon into the blood - substances essential for the endocrine process. Therefore, it is necessary to engage in the prevention of pancreatitis and its timely treatment.

Causes of chronic pancreatitis
Inflammation of the pancreas - this is pancreatitis. It can occur in an acute and chronic form, with the acute form implying the complete restoration of gland function with proper treatment, while the chronic form develops over the course of 10–15 years from the acute form and is characterized by a constant decrease in pancreatic function.
Chronic pancreatitis develops from an acute form of the disease. The reasons for it can be several factors:
- Regular use of alcohol in large quantities - this is the main cause in 50% of all cases of the disease. Enzymes, under the influence of alcohol, grow in the blood and stop in the vessels, and the sphincter spasm caused by the enzymes does not allow the enzymes to get to food and digest it;
- Eating large quantities of fatty or spicy foods with an unbalanced diet - attacks of acute pancreatitis usually appear after the holidays, when people eat a lot of unhealthy food and fill it with large amounts of alcohol;
- Gallstone disease - pancreatitis is its complication in 20% of all cases. Stones passing through the ducts block the enzymes in the ducts and do not allow them to reach the intestines, destroying the pancreas itself;
- Abdominal injuries or inflammatory processes in the abdominal organs;
- Infections - pancreatitis can be the result of viral hepatitis, mumps and even flu under certain circumstances;
- Metabolic disorders.
Any of the reasons listed above can be the beginning of acute and then chronic pancreatitis, so you should eat right, do not abuse alcohol, and be regularly monitored by a doctor.
Symptoms and diagnosis
Any disease has its own symptoms. The complexity of the symptoms of chronic inflammation of the pancreas in adults is that they appear for a while and then disappear.
Those. There are certain factors that excite the disease and manifest its symptoms.
You should be attentive to the body's reaction to certain factors in order to notice the trend in time and consult a doctor.
Symptoms of chronic pancreatitis are:
- pain of varying intensity in the left hypochondrium, sometimes radiating to the lower back. Attacks of pain usually occur after a meal and are permanent or temporary;
- nausea or vomiting;
- unpleasant belching, heartburn and persistent sour taste in the mouth;
- heaviness in the abdomen and constant rumbling;
- flatulence;
- frequent constipation, interspersed with loose stools;
- drastic weight loss.

Diabetes mellitus is often not only a concomitant disease, but also a symptom of pancreatitis. In the event of the occurrence, and even more regular appearance of one or more of the listed symptoms, you should consult a doctor for a diagnosis.
Allows you to identify it only special diagnostic procedures. The diagnostic process consists of several stages:
- Seeing a doctor and talking with him;
- Symptom detection;
- Visual examination of the patient, palpation and the detection of blistering or other abnormalities;

- Laboratory tests: blood, urine and feces;
- Coprogram - determination of the percentage of digested food;
- Taking specific and stress testing;
- Ultrasound;
- Gastroscopy;
- Endotropic sonography;
- Endoscopy.
In some cases, computed and magnetic resonance imaging is also performed. Since all the tests are quite specific, most often the patient is sent to the hospital immediately after visiting the doctor, where it is possible to take tests and carry out procedures in more favorable conditions and at the right time.
If the patient experiences pain, then the hospital is a prerequisite.
Inflammatory processes can occur in the connective tissues of the pancreas, its head, or the internal cavity, so full and complete research is necessary to identify the lesion and select the desired course of treatment.
Treatment of the disease
Pancreatitis treatment should have an integrated approach, the purpose of which will be the normalization and restoration of the gland. Treatment involves dieting and drug therapy. In special cases, surgery is prescribed.
The therapist is obliged to prescribe a strict diet, under which it is possible to prevent attacks of pancreatitis and its further development. Usually, a diet involves eating only boiled foods and steamed in minimal quantities.

Drug therapy is aimed at relieving pain. As medications used:
- No-silo - 1-2 tabl. up to 3 times a day;
- Novocain - prescribed by a doctor;
- Festal - up to 2 tablets 3 times a day;
- Mezim - 2 pills before meals and 2 pills after;
- Ampicillin is an antibiotic for the prevention of infection by 250-500 mg every 6 hours;
- Papaverine - 1 candle 2-3 times a day;
- Platyphyllinum - 2-4 mg up to 3 times a day;
- Promedol is prescribed by a doctor.
All medications used are usually referred to as antispasmodics, antisecretory and pancreatic drugs and should be used strictly as prescribed by the attending physician. The therapy should also include the elimination of alcohol dependence, if the cause of inflammatory processes in it and the active treatment of associated diseases.

Surgical intervention is prescribed in the case of a complex form of the disease, acute pain or the appearance of a cyst. Operations can be carried out in two ways:
- direct - removal of cysts and stones from the gland or complete removal of the organ;
- indirect - it includes operations on the bile ducts, intestines or neurotomy.
Can pancreatitis be cured?
The chronic version of pancreatitis implies irreversible changes in pancreatic tissues and is incurable. However, this disease is not fatal, with timely treatment. Patients who are diagnosed with this disease should:
- be seen by a doctor;
- be examined every 6 months;

- treat concomitant diseases;
- follow a diet;
- stop drinking alcohol;
- undergo a spa treatment.
You should not think that treatment depends only on the attending physician. Unfortunately, in chronic pancreatitis, his job is only to diagnose, relieve pain symptoms and prescribe diet and treatment.
Will the inflammation continue, depends only on the patient and his work on himself.
Diet for chronic pancreatitis
Diet is the most important item in the treatment of pancreatic inflammatory process. And it is also the most difficult, because it is not always easy to force yourself to eat simple porridge and refuse fatty and smoked. Diet for this disease implies:
- fasting in the first 2 days of painful attacks;
- total rejection of alcohol;
- maximum restriction of fat food;
- use only salt as spice;
- rejection of beans and cabbage;
- eating vegetables containing starch and fiber, only in baked or boiled form. These include potatoes, carrots, pumpkins, zucchini and beets;
- restriction of chocolate, cakes and cream cakes;
- rejection of coffee and carbonated beverages;
- use only warm foods, not hot;
- split meals;
- the use of vitamin complexes;
- rejection of strong broths and pickled products;
- the presence of foods high in protein;
- restriction of fats and carbohydrates.

It is compliance with the correct diet and the rejection of unwanted products, as well as a healthy lifestyle will help not only cope with bouts of chronic pancreatitis, but also reduce its negative effects to a minimum.
What to do during the exacerbation
Exacerbation of chronic pancreatitis means severe pain in the pancreas, possible vomiting and diarrhea. The first step in an exacerbation is to visit a doctor or call an ambulance at home. Pending the appearance of a medical professional, you should:
- To lie down - the patient needs complete rest;
- Do not eat either food or water;
- Put a heating pad with cold water on the left hypochondrium;
- Do not use painkillers.
In this position, you should wait for the doctor and then follow his recommendations. Since chronic pancreatitis has a period of exacerbation of several days, you should rest alone for 2-3 days (it is possible to take sick leave) and refuse food for a couple of days.

Complications and prognosis
Constant inflammation in the pancreas is characterized by the development of comorbidities such as diabetes, peptic ulcers and digestive disorders.
The mortality of chronic pancreatitis is about 20% in the first decade after diagnosis and 50% in the next 20 years.
Mortality is caused by the development of complications associated with the collapse of the affected pancreatic tissue and their entry into the blood. Exacerbations, digestive disorders and the development of infection also have a negative effect.
Development is possible:
- jaundice;
- acute renal failure;
- ulcerative lesions of the stomach;
- pulmonary edema and pneumonia.
With the rejection of alcohol, as well as with constant diet, the survival rate for patients with pancreatitis is up to 80%.
For more information about chronic pancreatitis, see the following video.