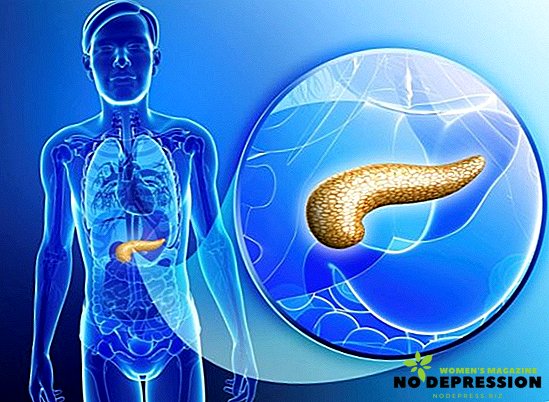
Pancreatic necrosis, or pancreatic necrosis, is one of the rarest diseases of the abdominal organs. In 70% of cases, the disease is diagnosed in young people. It can be either a separate pathology or a complication of acute pancreatitis. Chances to survive after the destruction of the pancreas are small, they range from 30 to 60% even with timely treatment. In case of total necrosis, the chances are zero.
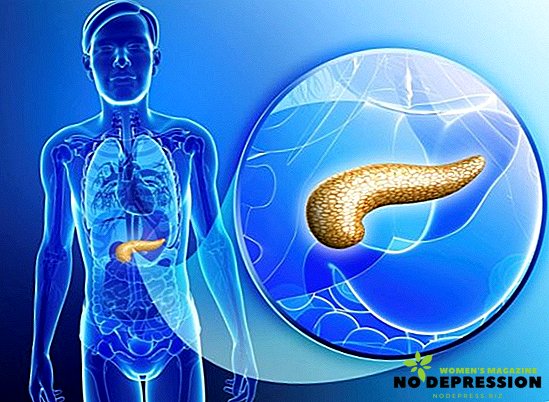
Pancreatonecrosis and its types
Pancreatic necrosis is a disease of the pancreas, in which cell death occurs as a result of the development of the inflammatory process. As a result, the gland is destroyed, its deficiency develops.
Pancreatic necrosis is often not a complication of acute pancreatitis, but one of its stages, characterized by a complex course and rapid progression.
Kinds
This pathology is classified by the following parameters:
- Depending on the prevalence of the destructive process, necrosis is: limited, widespread, subtotal (most of the gland is affected), total (the gland is damaged completely).
- By the presence of infections: sterile, infected. Sterile necrosis is divided into the following forms: adipose (manifests very slowly and in the first few days there is a positive prognosis for treatment) and hemorrhagic pancreatic necrosis (progressing very quickly, may be accompanied by internal bleeding).
- Depending on the course: progressive, abortive.
The main reasons for the development
Three main factors contribute to the development of this pathology.
The first of them - alimentary, is considered the most common cause of necrosis. In the body, destructive processes are triggered due to the consumption of significant doses of alcohol or large amounts of fatty foods. The second is an obstructive one. In this case, there is a blockage of the duct of the gland, which causes an increase in intraductal pressure, permeability of the walls of blood vessels, activation of gland enzymes - all this simply destroys the organ.
The third factor is called reflux: the reflux of bile from the duodenum into the pancreas is carried out. This activates the proferments and triggers some enzymatic reactions. In this case, the causes of necrosis are postoperative complications, abdominal injuries, endoscopic procedures, vascular vasculitis, sphincter disorder, food poisoning.
This pathology can occur in any person, but there is a risk group - categories of people with a high probability of developing this disease. These include patients with:
 chronic alcoholism;
chronic alcoholism;- gallstone disease;
- liver pathologies and pancreatic diseases;
- gastrointestinal diseases;
- congenital abnormalities of the digestive tract.
Mechanism of disease development
The basis of the pathology development mechanism lies in the disorder of the local protective forces of the gland. The development of necrosis occurs in three stages.
First phase
As a result of etiological factors, the external secretion of the pancreas increases, ducts stretch, and the outflow of pancreatic juices is disturbed. As a result of increased intraductal pressure, the parenchyma of the organ swells, small areas of the gland are destroyed, and the action of proteolytic enzymes is enhanced. All this leads to massive damage to the gland. Thus, the organs begin to digest themselves. When lipase is activated, the destruction of the vascular walls occurs.
Toxins or decomposition products of tissues and enzymes enter the bloodstream due to the destruction of the walls of blood vessels and have a toxic effect on all organs.
The liver, kidneys, heart and brain are affected. The development of any clinico-anatomical form of pathology depends on the predominance of the activity of lipase or elastase. If lipase is more active, the adipose tissue of the gland begins to collapse, then the necrotizing sites of the omentum, peritoneum, and internal organs begin to collapse. This form of necrosis is called fatty.
And in the case when microcirculatory disturbance prevails, vascular spasms occur, which causes rapid edema. In a few hours, the walls of the vessels expand and blood flow in the organs of the organs slows down. Such processes increase blood clots and subsequently lead to the appearance of ischemic necrosis. The increased effect of elastase leads to the destruction of the vascular walls of the gland, and then other organs.
As a result, the iron is soaked with blood, and hemorrhages develop in the internal organs, and effusion may appear in the abdominal cavity. This form of pathology is called hemorrhagic necrosis.
Second phase
An abscess forms in the pancreas and in the internal organs.
Third phase
In the pancreas and retroperitoneal tissue purulent processes develop.
Main symptoms of pathology
Necrosis of the pancreas has an obvious clinical picture. Due to this, this pathology is difficult to confuse with any other disease.
Pain
 The main symptom of this disease. Pain may occur in the left half of the abdomen, to give in the shoulder, back, groin. Often the patient cannot describe the exact location of the pain, it is also called shingles. The intensity of the pain syndrome is different, it depends on the severity of the pathology.
The main symptom of this disease. Pain may occur in the left half of the abdomen, to give in the shoulder, back, groin. Often the patient cannot describe the exact location of the pain, it is also called shingles. The intensity of the pain syndrome is different, it depends on the severity of the pathology.
The further the destructive process has progressed, the pain becomes less pronounced. This is due to the death of nerve endings. Reducing pain and the presence of intoxication are bad prognostic signs. The pain subsides somewhat in position on the side with knees bent. Therefore, patients with such pathology often take the described position to reduce discomfort.
Nausea and vomiting
Immediately after the onset of pain, unrestrained vomiting can begin. And it is not associated with eating, does not bring relief. Bile and blood clots are usually present in vomitus.
Signs of dehydration
Frequent vomiting leads to dehydration. As a result, the skin and mucous membranes become very dry, white scurf appears on the tongue, anuria may develop, when there is no urine output. A sick person constantly experiences thirst and dry mouth.
Flatulence and bloating
Since the pancreas is not involved in the digestive tract, the processes of decay begin to increase in the intestine. This causes increased flatulence, bloating, gas retention.
Signs of intoxication
These include:
- Toxemia. Toxins of bacteria that circulate in the blood lead to intoxication of the body. In this regard, the temperature may rise to 38 degrees and above, there is a general weakness, rapid heartbeat, breathing, shortness of breath, there is a decrease in pressure. The effect of toxins on the brain can cause encephalopathy. As a result, the patient's consciousness becomes confused, the state - excited or, conversely, inhibited. In severe toxemia, coma may develop.
- Hyperemia. During toxemia, the pancreas releases vasoactive substances into the blood, they dilate blood vessels. This is manifested by redness of the skin. With the subsequent development of intoxication, the skin turns pale, acquires an earthy or icteric color, becomes cold on the sides, on the back, buttocks, in the area of the navel may form blue-violet spots due to internal hematoma and hemorrhages.
- Internal bleeding. Due to increased elastase, blood vessels are destroyed, hemorrhagic effusions are formed in the abdominal cavity.
- Symptoms of peritoneal irritation. Stages of toxemia last about a week, characterized by an increase in symptoms, regardless of the intensity of treatment. The next stage is the formation of pus. Due to inflammation, the pancreas greatly increases in size, purulent infiltration is formed in the stomach. In the area of the pancreas, the skin becomes very sensitive, multiple organ failure may develop.
Possible complications
Complications of pancreatic necrosis include:
 peritonitis;
peritonitis;- abscess of the abdominal cavity;
- enzyme deficiency;
- a stomach or intestinal ulcer;
- fistulae
- pain shock;
- infectious toxic shock;
- suppuration in the pancreas;
- stomach attacks;
- portal vein thrombosis.
Diagnostics
The diagnosis of necrosis can be made on the basis of anamnesis and characteristic complaints, examination of the patient and additional examinations. Laboratory diagnosis includes a complete blood count. Due to dehydration, hematocrit, ESR, leukocytes, amylases, trypsin in the blood and urine, sugar and calcitonin in the blood increase, indicating severe inflammation or infection. An increase in C-reactive protein and an increase in liver enzymes are also observed.
Instrumental diagnostics includes:
- Ultrasound of the pancreas, biliary tract. With this pathology, concrements are observed in the biliary ducts, iron increases, a heterogeneous structure of organs is observed, fluid is present in the abdominal cavity, there are pockets of necrosis and cysts.
- Computed tomography also shows an enlarged gland, foci of necrosis, effusion in the abdominal cavity.

Also carried out an x-ray of the abdomen, MRI, puncture of fluid formations followed by bacposal material, the identification of possible microorganisms and the determination of their sensitivity to antibiotics, retrograde diagnostic laparoscopy.
How is the treatment?
After diagnosis, treatment must begin immediately. Patients are required to be hospitalized in the surgical department in the hospital, where complex therapy is carried out, aimed at suppressing the processes that occur, eliminating the symptoms and preventing the development of purulent complications. The sooner and more actively the therapy is started, the greater the chances for recovery. Treatment can be carried out by conservative or surgical methods.
Conservative therapy
It includes complete rest, bed rest and therapeutic fasting. During this period, the patient is prohibited any physical activity and eating. Food is parenteral for 5-7 days.
Pain suppression
For the relief of pain and relaxation of the sphincter, antispasmodic drugs are administered parenterally, for example, No-silo, Platyfillin, as well as non-narcotic analgesics, for example, Baralgin or Analgin. In addition, a regional Novocain blockade is acceptable. For severe pains, the administration of narcotic drugs with the exception of morphine is permitted.
Blocking pancreas and stomach secretion
To reduce the secretory activity of the stomach, anti-enzyme agents are administered intravenously, for example, Gordox. Suppression of gastric secretion is provided by the use of anticholinergics, for example, Atropine, as well as by washing the stomach with a special solution. It will also help reduce gastric secretion Omeprazole and other proton pump inhibitors.

In the absence of concomitant cholelithiasis, choleretic drugs are prescribed to unload the bile ducts. It is also necessary to provide local hypothermia, that is, put a cold on the stomach. This will not only help reduce the secretion of pancreas, but also ease the pain.
Antibiotics
Antibacterial drugs are prescribed for prophylactic purposes in case of aseptic necrosis, for suppressing pathogenic microflora, and for infection of the pancreas. Of the antibiotics, cephalosparins, for example, Cefepime using fluoroquinolones and metronidazole, are used.
Infusion treatment
To clear the blood of toxins and aggressive pancreatic enzymes, infusion therapy is prescribed. To fill the volume of fluid and improve the rheological properties of the blood, colloids, for example, Albumin, are injected intravenously. For the suppression of vomiting, Intramus is injected intramuscularly.
Infusion therapy is usually prescribed in combination with diuretic drugs, for example, furosemide to reduce edema and ensure forced diuresis.
Detoxification
Extracorporeal methods are used for detoxification: plasmapheresis, hemosorption, hemofiltration. The hormone of the hypothalamus is necessarily injected intravenously - it suppresses the secretion of gastric juice, endocrine functions. Also, this tool reduces blood flow in the internal organs, which helps prevent internal bleeding.
Surgical Therapy
In most cases, the development of this pathology shows the operation. The purpose of surgery is to determine the movement of pancreatic juices, remove necrotic foci, drainage of the abdominal cavity, stop bleeding.
Surgery may be postponed for several days until the patient’s condition stabilizes during acute pathology. But at the same time, immediate surgical treatment is indicated in the case of total necrosis, purulent peritonitis. In the presence of an infected destructive lesion of the gland, doctors prefer laparoscopic surgery - they provide wide access to the abdominal cavity.
Often during the events held specialists have to remove adjacent organs, such as the spleen, gallbladder. In some cases, reoperation is required due to the ongoing destruction of the pancreas. Radical surgical treatment involves the removal of necrotic masses, parts of an organ or organ completely.
In case of necrosis, it is recommended to perform minimally invasive surgeries, such as laparoscopic reorganization, drainage of the abdominal cavity.
Rehabilitation features
After the operation, the patient’s disability may persist for 3-4 months or more. In the postoperative period, recovery of the patient depends on the care and rehabilitation measures. In the first three days, the operated patient should be in the intensive care unit, where experts monitor pressure, electrolyte levels, sugar, demritis, urine values.
With a stable condition, the patient is transferred to the general surgical ward. The first two days shows therapeutic fasting. Three days after the operation a sparing diet is allowed:
- unsweetened tea;

- shredded liquid soups in vegetable broth;
- buckwheat and rice porridge on the water;
- protein omelette;
- cottage cheese;
- butter;
- at night you can drink a glass of yogurt or warm water with honey.
In the first 10 days after the operation, all dishes are steamed, then boiled lean meat and fish in small quantities can be added to the ration. Discharge from the hospital takes about one and a half to two months.
Home treatment
In the first few days after discharge the patient is recommended bed rest. Obligatory dieting, afternoon nap is mandatory. After 2 weeks, small outdoor walks are allowed, the duration of which can be gradually increased.
It is very important not to overwork during the rehabilitation period. Reading, watching TV, small household chores should stop as soon as the patient begins to feel ill.
Rehabilitation activities include:
- taking insulin-containing drugs for the regulation of blood sugar;
- multienzyme preparations for the assimilation of food;
- Physiotherapy and physiotherapy.
Features of nutrition after surgery
For pancreatic necrosis, there are several recommendations for dieting:
- meals should be fractional, in small portions, about 6 times a day;
- it is desirable to take food at the same time;
- it is necessary to completely eliminate smoking and alcohol;
- dishes should be at room temperature;
- food is desirable to grind;
- dishes can be steamed, stewed or boiled.
Forbidden products include:
 fresh bread;
fresh bread;- pearl barley;
- corn grits;
- beans;
- lentils;
- fatty meats and fish;
- coffee, chocolate, strong tea;
- canned food, smoked meats, sausages;
- pickles and pickles;
- mushrooms and mushroom broth;
- meat or fish broths;
- white cabbage;
- sour or spicy vegetables;
- lard, margarine, animal fats;
- whole milk and fatty dairy products;
- eggs;
- grapes, dates, figs.
You can consume:
- low fat cottage cheese;
- vegetable soups;
- porridge on the water or milky water mixture;
- boiled pasta;
- lean fish and meat;
- boiled vegetables;
- butter;
- savory dry biscuits;
- diluted fresh juices.
What are the predictions?
With this pathology, the prognosis is doubtful and depends on many factors: how quickly treatment was started, the patient's age, the form of the pathology, the presence of concomitant diseases, compliance with medical recommendations, the extent of surgical intervention.
Diabetes can develop in 25% of patients who have suffered a destructive form of pancreatitis. Pseudocysts are often formed, chronic pancreatitis can occur, and pancreatic fistulas appear. Mortality in this pathology is very high - in the case of septic necrosis it is up to 40%, with an infected - 60%.


 chronic alcoholism;
chronic alcoholism; peritonitis;
peritonitis;
 fresh bread;
fresh bread;