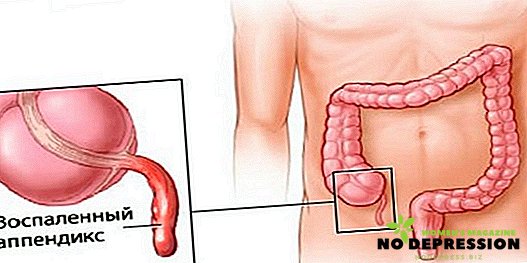
Chronic pancreatitis is a progressive pathology of the pancreas, having an inflammatory nature. During exacerbations, pain in the hypochondrium, nausea, vomiting, abdominal distension, and yellowness of the skin may appear. In the absence of proper treatment, this disease can lead to serious complications, including death.

What is chronic pancreatitis?
Chronic pancreatitis is an inflammatory disease of the pancreas of a long course, characterized by gradual pathological changes in the cellular structure of the body and the development of functional failure.
With the progression of the disease in the gland, the secretion of enzymes decreases, which is why the blood circulation of the organ deteriorates, connective tissues grow, which leads to the formation of scars.
Usually this disease occurs with prolonged use of alcohol. In men, pathology can develop when alcohol is consumed over a period of 15 years; in women, it is faster in 10-12 years.
Causes of development
The main mechanism of the development of the disease is to increase the pressure in the pancreatic ducts, the stagnation of gastric juice. This causes a violation of the structure of the ducts, because of which the enzymes of the biliary gland begin to penetrate into their own tissue, which leads to the development of the inflammatory process. This process may take about 15 years.
The main reasons for the development of this pathology include the presence of:
- cholecystitis, gastritis;
- stomach ulcers;
- infectious lesions (for example, viral hepatitis, mumps);
- alcohol addiction;
- atherosclerotic disease;
- parasites (worms).
Stages of development of the disease:
| Stage pathology | Description |
|---|---|
| Easy | During this period, the first signs begin to torment, and the duration of this stage can last for 2-3 years. In the presence of provoking factors, the disease can develop rapidly. About 1-2 exacerbations can be observed per year. |
| Average | At this stage, symptoms of endocrine insufficiency appear. During this period, patients eat little, constantly complain of abdominal pain. There is a year of up to 4 exacerbations, and they occur in a more severe form. There is a decrease in body weight. |
| Heavy | At this stage, there are regular and long-lasting attacks with intense and pronounced symptoms. Weight decreases, diarrhea can begin. Additionally, complications such as diabetes mellitus or intestinal stenosis may occur. |
Symptoms of the disease
Often, the initial changes in the tissues are almost asymptomatic or they are mild. But in the event of the first exacerbations, one can say that the pathological disorders are already quite impressive.
The main features of this disease include:
 Pain syndrome of different intensity. Most often, the pain is localized in the left hypochondrium.
Pain syndrome of different intensity. Most often, the pain is localized in the left hypochondrium.- Dyspeptic disorders that are accompanied by nausea, vomiting, feeling of heaviness in the stomach, unpleasant taste. A large number of patients there is aversion to fatty foods or lack of appetite.
- Over the years, a person may complain of pain symptoms that bother him for 15-30 minutes after eating. The feeling of discomfort may not go away for 5 days. Localized pain at the top of the abdomen, sometimes pain can be felt near the heart or lumbar region.
- The skin turns yellow, and the yellowness can pass with time.
Due to the lack of enzymes in the pancreas, the process of splitting the complex molecules of food consumed, which are absorbed in the intestine, is disturbed. Because of this, with pancreatitis, even with intensive nutrition, weight can quickly decrease, there will be a lack of vitamins, dry skin.
If we talk about the chronic form of the disease, then during this period pain occurs due to:
- problems with the outflow of pancreatic fluid;
- ischemia of the pancreas;
- deformations of nerve endings;
- inflammatory process;
- squeezing nearby organs.
With the development of the disease, the frequency of exacerbations increases. Chronic inflammation of the pancreas can cause damage to the gland itself or to nearby tissues.
Exacerbation of pathology
Exacerbation of the disease can be caused by two reasons:
- intake of a large amount of alcoholic beverages;
- violation of the biliary tract.
There are also other reasons that, although of lesser importance, can significantly increase the frequency of exacerbations:
- binge eating;
- overweight;
- consumption of large amounts of fatty foods;
- medication;
- infectious diseases;
- regular stress.

In most cases, signs of exacerbations are manifested in the form of severe pain, which is localized under the ribs and gives back. In some cases, the pain gives to the side, in the chest.
The characteristic signs of aggravation include:
- severe pain in the abdominal cavity, which increases after eating;
- frequent bouts of diarrhea;
- feeling of bitterness in the mouth;
- vomiting that is difficult to suppress with medication;
- loss of appetite;
- the appearance of white bloom.
Complications
If time does not cure pancreatitis, it can cause the development of such complications as:
- pancreatic ascites;
- diabetes;
- abscess;
- inflammatory processes in the excretory ducts;
- portal hypertension;
- bleeding in the gastrointestinal tract;
- the appearance of tumors.
How is the diagnosis
Therapist or a gastroenterologist may be involved in the treatment of this disease, in the presence of endocrine insufficiency, an endocrinologist should be consulted. If adjacent organs are damaged or constricted, contact a surgeon.
The diagnosis will be made only after all the studies:
- analysis of the content of elastase in urine;
- analysis for the detection of sweaters;
- iron stimulation tests;
- Ultrasound;
- CT scan;
- glucose analysis.

Treatment of chronic pancreatitis
The main goals of therapy are as follows:
- pain relief;
- pancreas dormancy;
- a decrease in the secretory activity of the gland;
- fill the shortage of pancreatic enzymes;
- if necessary, correction of impaired carbohydrate metabolism.
The best treatment is complex, including various methods of therapy.
Medication
With this pathology is usually prescribed:
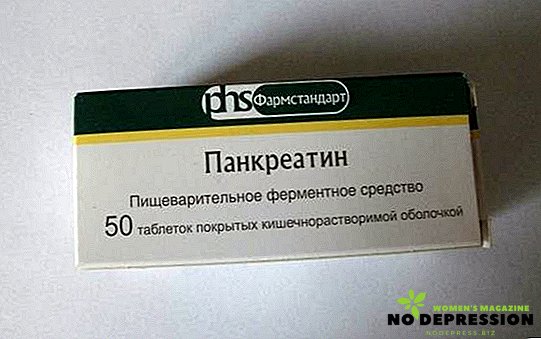
- Enzyme-containing drugs that are aimed at reducing the load on the body, accelerating tissue regeneration. Digestive enzymes will help facilitate the process of digestion, digestion of food, the work of the digestive tract. As a result of their regular intake, appetite appears, nausea disappears. The most popular drugs of this group are: Creon, Pancreatin.
- Antacid drugs aimed at reducing acidity. By the principle of impact, they are divided into nonabsorbable ones, which envelop the stomach (for example, Almagel), and suction - Rennie. Absorbable remedies provide quicker relief, but the effect is short. A non-absorbable, though they begin to act after a while, but they have a longer effect.
- Analgesics that help reduce pain during exacerbations. When spasms appear, spasmolytics are prescribed, such as Papaverine or No-silo.

- Antisecretory drugs are prescribed to neutralize the action of the acid. The most famous drug in this group is Omeprazole.
- Anti-inflammatory drugs are prescribed to reduce pain and reduce inflammation, for example, Diclofenac does well.
- In periods of exacerbation, drugs such as Sandostatin or Octreotide are prescribed to reduce the active secretion of the gland. They are also effective in marked pain syndrome when antispasmodics do not help.
- To suppress the feeling of nausea or vomiting during the exacerbation of chronic pancreatitis, prokinetics, such as Zerukal, should be taken.

Exacerbation therapy
Treatment for severe exacerbation consists of adherence to bed rest, proper diet, medication, but only in the hospital, because during such periods there is a threat to the patient. In case of exacerbation of the disease, you need to call an ambulance, put ice on the abdomen before the arrival of the brigade, ensure complete rest and hunger.
Most often, the duration of a chronic attack does not exceed 7 days.
As ancillary drugs for the relief of pain use:
- enzymes, such as Creon;
- antispasmodics: Drotaverine;
- proton pump inhibitors: Lansoprazol.

To relieve the pancreas, you need:
- completely exclude smoking and alcohol;
- stick to a diet;
- take the drug Octreotide.
Surgical intervention
Operations for chronic pancreatitis are carried out in such cases as:
- sphincterotomy for blockage of the sphincter;
- incidence of stones in the pancreatic ducts;
- complete or partial pancrectomy;
- the formation and dissection of purulent foci;
- resection of the stomach.
Folk remedies
There are many popular methods of treatment of this disease. Below are the most effective.
To prepare a healthy broth, you need the following ingredients:
- 10 g of chamomile drug;
- 30 g of dill;
- 20 g hawthorn red;
- 20 g immortelle;
- 30 g mint.
 We grind all herbs, we mix, we take 2 tablespoons. collection, pour 0.5 liters of hot water and leave to infuse in a thermos for about 3-4 hours. Take need to 100 ml of broth an hour after a meal. The tool has antispasmodic, antimicrobial, choleretic action.
We grind all herbs, we mix, we take 2 tablespoons. collection, pour 0.5 liters of hot water and leave to infuse in a thermos for about 3-4 hours. Take need to 100 ml of broth an hour after a meal. The tool has antispasmodic, antimicrobial, choleretic action.
Another effective remedy consists of 50 g of dandelion root and calamus and 25 g of thyme, nettle roots, hop cones.
All grind in a coffee grinder, mix 5 tbsp. collection with 200 g of honey. Take need for 2 tsp. twice a day for a month.
Diet and nutrition
Nutrition needs to be given special attention, because a proper diet can alleviate the patient's condition. This is very important because each attack of exacerbation causes the replacement of healthy fibrious tissue, which ultimately leads to the development of gland insufficiency.
In chronic pancreatitis, it is advisable to follow the diet number 5. In this case, in the diet you need to enter more protein foods, but carbohydrates or fats should be tried to completely eliminate. Also, with such a diet should be abandoned fatty meats, plant foods.
Meals should be fractional, in small portions 5-6 times a day. To eliminate the likelihood of relapse, you should completely give up alcohol.
Other recommendations:
- New products should be introduced into the diet in small doses, if they are not healthy, they should be abandoned until normalization of the pancreas;
- It is advisable to chew food thoroughly, even if you eat cream soup.
Despite some limitations, diet No. 5 with this pathology is quite diverse:
 lean meat and poultry;
lean meat and poultry;- lean fish boiled;
- vegetarian soups;
- wiped boiled vegetables;
- omelets;
- low-fat dairy products: cottage cheese, sour cream, cream in moderation;
- cookies without sugar, crackers from white bread;
- cereals (on water or on water and milk in equal proportions);
- black tea with lemon, compotes;
- baked apples, grated berries;
- boiled macaroni.
But fried foods, meat and mushroom broths are forbidden with such a diet.
During remission, the list of products expands: you can include raw vegetables and fruits, adding them to cereals, salads; dried fruits; cereals; not mashed soups. Also, as a preventive measure, you need to drink mineral water (for example, Borjomi, Essentuki No. 4) within a month.
Acceptance of mineral water during this period is due to the fact that it:
- prevents stagnant processes both in the pancreas itself and in its ducts;
- reduces the risk of inflammation;
- normalizes the digestive tract.
Preventive measures
Prevention of the development of chronic pancreatitis includes:
- quitting smoking and drinking alcohol;
- dieting;
- regular passing of routine inspections by narrow specialists.
In addition, when the first signs of pathology appear, an urgent need to consult a doctor is not self-healing.


 Pain syndrome of different intensity. Most often, the pain is localized in the left hypochondrium.
Pain syndrome of different intensity. Most often, the pain is localized in the left hypochondrium.



 lean meat and poultry;
lean meat and poultry;